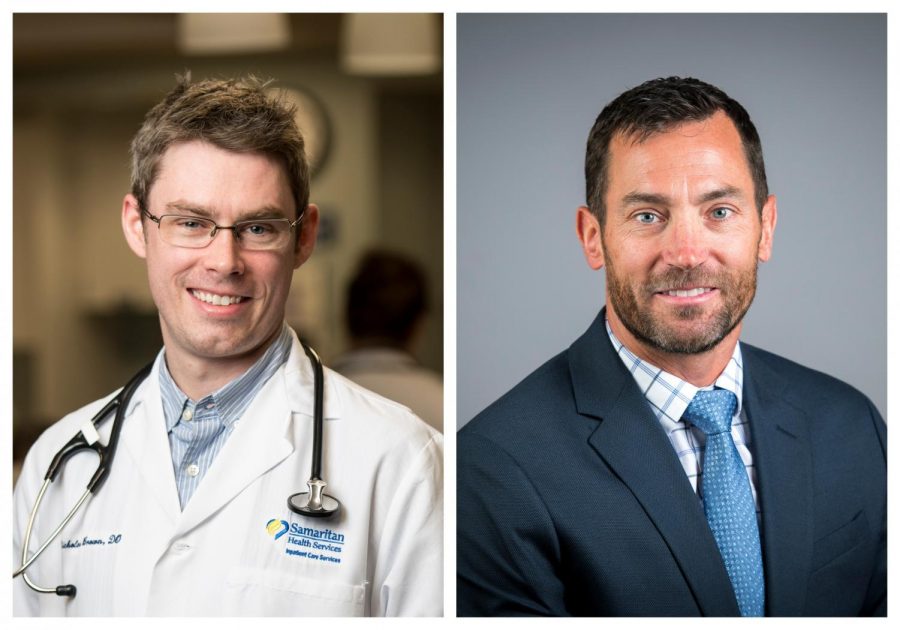
Nicholas Brown and Brian Delmonaco: Fighting COVID-19 on the front lines
April 20, 2020
This Q&A is the eleventh in a 19-part series, “19 COVID-19 Stories,” updated on Mondays, Wednesdays and Fridays, diving into the unique perspectives of the Corvallis community as they face COVID-19 and all its social and economic effects. The Baro spoke with two local doctors, Dr. Nicholas Brown and Dr. Brian Delmonaco, to find out what it’s like working in a hospital during the COVID-19 pandemic.
Dr. Nicholas Brown, a hospitalist medical director, has worked at Good Samaritan Regional Medical Center in Corvallis, Ore. since 2011. During his first three years, he completed his training as a resident physician, and has since joined the hospitalist group as a provider. He began his current position as medical director this past year.
What is your job like on a day-to-day basis, prior to COVID-19?
I spend about half of my time seeing patients only in the hospital, the other half doing a combination of resident education as an academic physician and managing our group of 26 hospitalists. These physicians cover the patients in the hospital 24 hours a day, every day of the year. To make this possible, we have daytime hospitalist coverage and nighttime hospitalist coverage. Each shift is 12 hours. A typical day or night shift for us is busy and everyone can expect to be busy seeing patients or involved in care for the entire day.
How has your job changed since the arrival of COVID-19?
Personally, as a group leader, there has been a lot of administrative tasks and projects put on hold while focusing all our efforts on preparing for and caring for COVID-19 patients. As a clinician there is a much higher awareness of the risk of our jobs. We have always had risks: caring for any patient with a communicable disease, such as influenza, would put us at risk, however we are certainly much more aware of the risk now. That said, we’ve got this. We know how to use personal protective equipment, we know how to care for patients with respiratory illnesses.
What new procedures or protocols have been enacted in your workplace since the arrival of COVID-19?
There have been many changes with regard to the use of personal protective equipment, such as wearing masks throughout the workday. That is obvious. But there are other big changes: typically, we expect to talk with patient’s families in person while their loved one is hospitalized, however currently we have visitor restrictions. Therefore, we are spending much more time on the phone to communicate clearly with families. We have started using video apps like FaceTime for patient care to reduce the number of trips into a patient room and use of personal protective equipment.
What have been the biggest challenges or most difficult aspect of the COVID-19 outbreak for you, both as an individual and as a medical professional?
As an individual, it has been concerning for my own family while social isolating, because I know that if they became ill, it would most likely be because of contact with me. That has been a common concern among medical providers, though. As a medical professional, it has been the rapid pace of change. There are a lot of changes to policies, procedures that we all must keep up on and inform each other. Being adaptive is currently critical, because what we did yesterday may be different today. But also keeping up with rapidly changing information in regards to COVID-19. There isn’t much else in the news right now, therefore everyone is getting a lot of information, not all of it is accurate, and we must continue to educate ourselves and others on what is scientifically known about COVID-19.
What has been the most uplifting aspect of the outbreak?
Two things come to mind immediately, teamwork and community. Our team at GSRMC, including everyone at every level, has been incredibly supportive of one another, working diligently to adapt to these rapid changes and stressful situations. Our community as a whole have been incredibly supportive of the healthcare workers, and every effort they have personally made to social distance and flatten the curve has thus far been effective for our region.
Anything else you’d like to add?
I’m thankful every day that I get to work in such an amazing community and with a great organization.
Brian Delmonaco, MD, a pulmonologist and leader of the intensivist team at Good Samaritan Regional Medical Center in Corvallis, Ore., specializes in critical care and emergency medicine. Delmonaco has worked at GSRMC for approximately 12 months, joining the team with prior experience in intensive care and emergency medicine.
What is your job like on a day-to-day basis, prior to COVID-19?
My profession and career are the best in the world. I care for the sickest people on the planet and help them and their families through the journey of severe illness. This has not changed since COVID-19; however, the communication channels have changed due to concern for visitors’ safety from spread of coronavirus. Virtual visits are much more common than prior to the pandemic.
How has your job changed since the arrival of COVID-19?
We have many procedures and protocols that, though they existed prior to coronavirus, are used more frequently. For example, personal protective equipment has not changed—but we have many more opportunities to don it. Our tempo for collaboration increased by a power or two—collaboration among colleagues throughout Samaritan Health Services as well as the state of Oregon, nationally and internationally. Prior to COVID-19 from time to time, we deployed therapies that were not rigorously supported by double-blinded randomized controlled trials (RCTs) or evidence-based research—with COVID-19 there are no RCTs and we must use our best judgement while we develop evidentiary medicine.
What have been the biggest challenges or most difficult aspects of the COVID-19 outbreak for you, both as an individual and as a medical professional?
COVID-19 impacts everyone in my family. My elderly parents are getting groceries delivered to them. My son has no swimming pool in which to train. My wife is a nurse in the emergency department and is at the tip of the spear in the fight against COVID-19. The biggest challenge as a medical professional is the lack of definitive knowledge of the source of the SARS-CoV-2 virus, its pathophysiology, its definitive treatment or prevention. Once we know its definitive source, for example, we can begin to identify the pathophysiology that is unique to this virus followed by a recognition of who is most vulnerable and how to save them.
What has been the most uplifting aspect of the outbreak, if any?
The most uplifting aspect of the outbreak has been the collaboration and teamwork between the engineers at H-P, the scientists at OSU and the medical professionals at Good Samaritan Regional Medical Center at a breakneck speed to help treat critically ill patients and keep hospital and clinic staff safe. Our community is stronger because of our perseverance and dedication.