Concussion evaluation
February 13, 2017
As the NCAA continues the biggest concussion study in history, OSU continues to evaluate concussion protocol and its support system
Hayden Craig’s fifth and final concussion happened in practice, as many concussions do.
It was the 2014 spring football season. During one play, Craig got hit on the side of the head, blacked out momentarily and lost all memory for about a 40-minute period. Still, Craig got up and was able to go through the motions on the next two plays before anyone, including Craig himself, realized how hurt he was.
The NCAA started releasing results last week from its nearly three-year concussion study that have noted the danger of concussed players returning to
action too quickly.
In May 2014, the NCAA and the U.S. Department of Defense launched a nationwide concussion study called the Concussion Assessment, Research and Education (CARE) Consortium study. It enrolled more than 28,000 participants across 30 universities, making it the largest concussion study ever conducted. The preliminary findings were released on Jan. 31 in a concussion conference hosted at UCLA by the Pac-12 Conference, though much more analysis and data will be released within
the next year.
According to the NCAA’s release, researchers hope the study lays the foundation for a “decades-long examination of the long-term effects of concussion and exposure to contact.”
Of those 28,000 student-athletes enrolled, 1,600 concussions were recorded with nearly 300 coming specifically from football practices and games.
Compared to a 2001 concussion study—then the largest of its kind—concussed athletes returned to play an average of 6.7 days after injury. That average is now up to 14.3 days. In the 2001 study, 92 percent of repeat concussions happened within 10 days of the first injury. Compare that to this NCAA study, which didn’t report a single repeat concussion within 10 days despite the larger scope.
While the drop from 92 percent to zero is momentous, there still exist areas of improvement. Athletic departments like OSU’s have to answer a big question—how do you protect student-athletes who get a concussion and don’t tell the trainers?
Dr. Doug Aukerman, OSU’s senior associate athletic director for sports medicine, is trying to help answer that question. As the primary day-to-day manager for OSU’s entire sports medicine program, handling concussion protocol is one of his
biggest responsibilities.
One way that Aukerman, OSU and other universities have been trying to prevent situations like Craig’s is with a test called EYE-SYNC. A potentially concussed athlete straps on the EYE-SYNC goggles and has to track a moving dot on the screen with their eyes for about 30 seconds; the results can show if a player is struggling to focus, which is a key symptom of concussions. Theoretically, EYE-SYNC can objectively and quickly show if a player is exhibiting concussions symptoms, even from the sideline of a football game. OSU has started using EYE-SYNC during football games and practices this last fall.
The credit for EYE-SYNC goes to Stanford’s Concussion and Brain Performance Center, but OSU is one of the schools that has been using the method to collect data. Aukerman says that EYE-SYNC could be ready to be used on a widespread basis immediately once the data collection phase is completed, which he estimates would be within the next year.
“It’s an objective measurement,” Aukerman said. “Otherwise you really are heavily dependent on the student-athlete being honest, coming forward and providing information of their symptoms they’re experiencing. And it’s really the job of the athletic trainers, coaches and other support staff to keep their eyes out, and if they see signs of a student-athlete having a concussion, that they step in and try to get them evaluated.”
Another way OSU and other schools have attempted noting concussions quickly is with a medical spotter, which every Pac-12 team started using for football games starting in 2015. OSU’s medical spotter sits in the press box and alerts coaches and medical staff on the field if they notice an injury that wasn’t initially reported. The spotter watches a live video feed of the game and can rewind, pause, zoom and change camera angles to evaluate players for possible injuries.
Beyond Eye-SYNC and the medical spotters, another aspect of concussions is the continued collisions a player expreriences throughout a season.
“I do see from personal experience, a lot of concussions come from scout team,” Craig said. “Your risk gets higher, and this happens all the time, when the scout team runs a play and the defense doesn’t run it right. (Coaches) tell you to run it again, and obviously they know where the play is going and sometimes the kid gets popped a little bit harder than needed.”
OSU now uses Guardian Caps in football practice, a seven-ounce foam padding attached to the outside of football helmets. Its creator, Guardian Innovations, says the modified polyurethane caps can absorb up to 33 percent of an impact. OSU was one of the first major Division-I football programs to use Guardian Caps.
Noting how football players can take hundreds of collisions and “sub-concussive blows” over a season. Aukerman proposed the idea to OSU’s staff in 2015 as another way to limit student-athletes’ exposure to repeated head trauma. Players are not required to wear the padding, but interior linemen are the
most common users.
Because of how debilitating the symptoms of concussions can be, returning student-athletes to the playing field and the classroom can be difficult.
During last football season, OSU senior cornerback Treston Decoud talked in an interview with Barometer about his concussion in the game against Colorado in October 2015. Decoud blacked out after colliding with a teammate, remained unconscious for about six minutes and was taken immediately to the hospital. Decoud returned to the locker room by the game’s end, but was so fuzzy afterward that he showed up to practice the next day even though the team had the day off.
Decoud also went to class the next day thinking it was Tuesday, taking him several minutes in the empty classroom before realizing he was in the wrong place. Around the same time, Decoud saw assistant football coach Mitch Singler and didn’t even recognize him. Singler had to tell him about the encounter later, which Decoud had no memory of.
“It was a blurry time in my life,” Decoud said. “It was like my head was in a whole different place. It was scary. I swear to God it was scary. I used to cry every night because my head was hurting. I couldn’t watch TV, I couldn’t do nothing. Any light or noise made my head hurt. It was a bad two weeks.”
Craig has seen similar issues firsthand, and not only in his own experience. He recalls watching an injured teammate try to walk off the field to the locker room, but was too severely concussed to remember the door code. He kept on hitting the handle, unable to figure out how to get in.
“Concussions—they mess people up,” Craig said.
Craig’s case was no different. After being escorted to the locker room, he began vomiting in a downstairs bathroom and needed his roommate to come pick him up.
It’s circumstances like this that led OSU to its concussion management plan, a 10-page document outlining basic procedures including the Return to Play and Return to Learn guidelines, which cover the process by which student-athletes can return to the playing field and to the classroom, respectively.
Concussions can hold student-athletes off the field, but also the classroom. Craig experienced this first hand.
“It was miserable being in a classroom,” he said. “And that’s how a lot of guys are with concussions.”
The plan is meant to ensure the athletic department, medical staff and academic faculty are on the same page when a student-athlete gets a concussion and might need special accommodations.
OSU relies on its Faculty Athletic Representative (FAR) to be the liaison between the athletic and academic departments, also working with the team physician, professors, academic counselor, the Office of Disability Access Services and others.
OSU’s FAR, Joey Spatafora, gets involved once a student-athlete has missed about a week of class and might need help.
Last year Spatafora worked with a student-athlete who got a concussion and wasn’t able to return to class. Since the student-athlete couldn’t go to class for three weeks, Spatafora helped them withdraw from class without academic or financial penalty.
“There’s a lot of things you have to do to petition for that,” Spatafora said. “My role was helping the student understand the policies and procedures that would have to be followed to get that relief, and it worked out well.”
Craig has a similar story, noting that athletic trainers Stephen Gaul and Ariko Iso were “awesome” in walking alongside him in the concussion protocol. He also pointed to the academic counseling staff as being particularly helpful.
“Thank God Oregon State has a good protocol with the university,” Craig said. “I think they have great avenues to help student-athletes in need not fall behind in school. They take care of them. I would say the relationship between the athletic department and the student health organization within the school is on the same page. If a student had a concussion, he’s not going to be in the class and the teachers are okay with it. They understand.”
Spatafora has been OSU’s FAR for the last seven years, but the Return to Learn procedure was formalized by the NCAA two years ago.
Craig’s concussion was back in 2014, so OSU now has an even more thorough framework, as Aukerman says, that specifies which people should get involved if a student-athlete needs aid. Aukerman says the biggest change in OSU’s concussion protocol he’s seen in the five years he has been at the university has been the Return to Learn plan the NCAA outlined. Until it was implemented two years ago, focus was more on the physical prevention and recovery of concussed athletes but not as much on the academic support that injured student-athletes need.
“(The NCAA) forced a lot of university institutions to start paying attention to that component of concussions, whereas before there wasn’t a lot of attention paid to it
necessarily,” Aukerman said.
Seriously concussed athletes like Craig simply don’t have the mental capacity after their injury to handle their normal academic load.
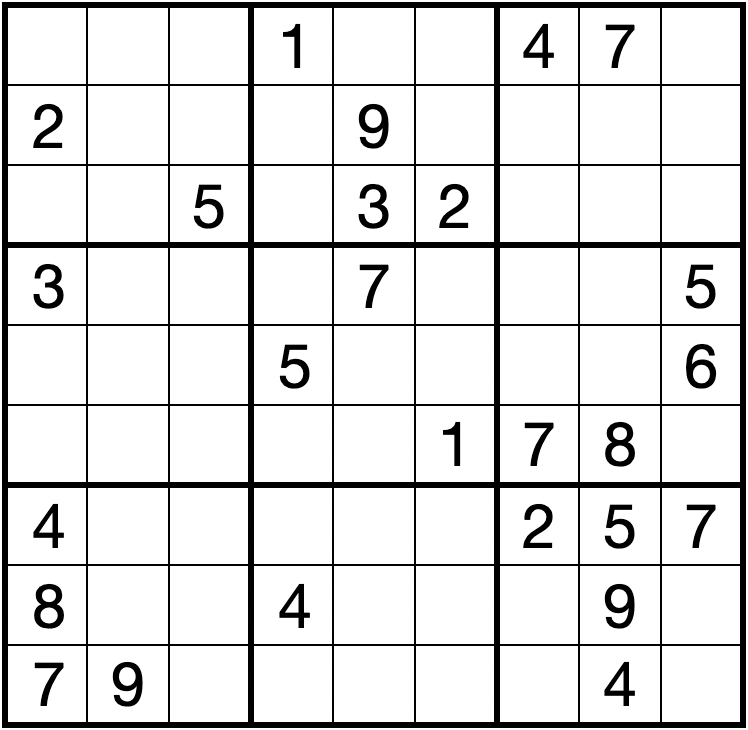
“You can look at a board and see two plus two. Well, any normal person can look at it and say, ‘Two plus two is four,’” Craig said. “I sat there, looked at it, thought for a second and said, ‘Oh, it’s four.’ That quick-trigger is not there.”
OSU’s concussion management procedure also includes a rule that any concussed student-athlete must be given an overnight contact to monitor the injured athlete over the next 24 hours. Often a roommate, friend or significant other, the overnight contact is given an instruction form that includes warning signs that the athlete might need immediate medical attention.
For the most serious of concussions, an overnight contact can be instrumental. Decoud, for instance, had trouble just getting back to his apartment after his concussion without the help of teammate Devin Chappell.
“I remember walking him home, him leaning on me and I’m carrying him on my shoulder,” Chappell said in an interview with the Barometer last fall.
Decoud recognized the importance the overnight contact had carried for him.
“Thank God for Devin Chappell,” Decoud added. “He had me. If he hadn’t helped me, I don’t know if I would be still here. That concussion was bad for me. I still think about that.”
The final step of concussion management, and perhaps the most difficult, is discussing the possibility of medical retirement. When Craig was deciding in 2014 between retiring and trying to come back, he knew his long-term health was on the line.
“I was taking a huge chance if I decided to play again, so that was the main focus,” he said. “I made a decision at the age of 20 to no longer play, which was a really mature decision of mine that you don’t see kids at that age making. I’ll tell you this, there’s a lot of kids on that team that never should have been playing. But they had to because that’s all they had.”
Craig touches on a point that coaches and doctors alike have to deal with. It’s one thing to inform a student-athlete of all the risks of continuing to play a collegiate sport after they’ve received a concussion. But if that student-athlete doesn’t feel they’ve got anything to go to if they retire, what then?
“It’s a discussion we have over multiple visits over a period of time,” Aukerman says about breaching the topic of retirement. “It’s not something we say all of a sudden, ‘Okay, you’re done.’ Because there’s no question there’s a psychological component to not playing a sport that you’ve played for a long time. How do you make that transition in a healthy way, especially if your identity was tied to that sport? So we have to be aware of that process of moving out of a sport that has been such a huge part of your life up to that point.”
Craig’s position coach, Tavita Thompson, was even more firm. When talking with Craig, he was straight-forward: “If you were my child,” Thompson said, “I would not let you play football anymore, so I’m not going to play you even if you decide to play.”
To this day, Craig says his decision to retire three years ago was the right choice. Even while retiring as soon as he did, he still has some medical issues he deals with today like occasional slurring of words, sensitivity to light and diminishing eyesight, which Craig says has forced him to get glasses for the first time.
“With the amount of concussions I had and the severity of them, my new 100 percent is not what the old 100 percent was,” Craig said. “Now, 96 percent is my 100 percent.”
For those involved in OSU’s concussion protocol like Aukerman and Spatafora, helping student-athletes go through difficult decisions like Craig’s is their job. Most importantly, they say, their goal in helping student-athletes recover from brain injuries is about more than just getting them back to the field.
“The majority of our student-athletes are not going to become professional athletes,” Spatafora said. “We want them to have as rich of an experience as possible athletically, because for most of them, this is it. This is the peak of their athletic competition. But we want to protect them. Like all groups of students, they’re unique. They’re really at the peak of their game with respect to their athletic career. We want to protect them, put them in a position to succeed (athletically), but also succeed academically because that’s what they’re going to be doing the rest of their life.”