Indra Lab advances dermatology research
April 9, 2018
3D skin generation technology replaces human testing.
Beyond the double doors of the Oregon State University College of Pharmacy, the murals paying homage to classic and modern medicine and a few classrooms, lies the Indra Lab.
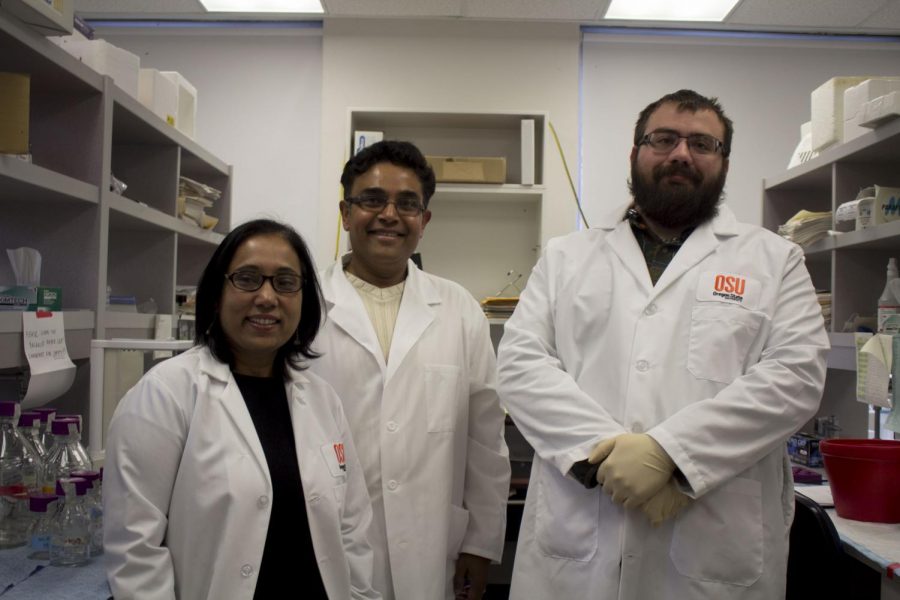
Led by associate professor Arup Indra and associate professor Gitali Indra, the Indra lab is a joint effort to attack major issues in dermatology.
After bringing the dermatology to campus for the first time in 2005, the Indras have developed extensive collaborations in the college and with different colleges on campus, and are now collaborating with researchers and clinicians at OHSU and Knight Cancer Institute in Portland.
“There are three major projects we work on. One is on inflammatory skin diseases such as eczema,” Arup Indra said. “The second is there is work on melanoma and the third is skin regeneration and wound healing.”
The third pathway of research in the Indra Lab involves melanoma, or skin cancer, research. Melanoma can prove to be fatal, and Oregon has the 3rd highest incidence rate of it, according to Indra in a March 5 Baro article.
Eczema
According to Arup Indra, eczema is a widespread condition in the global community. “Essentially, eczema is an inflammatory disease that affects almost 10 percent of the world’s population,” Arup Indra said. “It affects both pediatric populations as well as adults any age.”
Eczema is a broad term to describe skin inflammatory diseases, Arup Indra said. His group specializes in studying one subgroup known as ‘atopic dermatitis,’ translated to any reaction found on the upper layer of the skin, or the epidermis.
“The skin acts as a barrier between the environment and our body. So that means that the skin helps to keep the inside in and the outside out,” Arup Indra said. “And if you believe me or not it’s the largest organ in the body. And the epidermis gets regenerated every two weeks.”
When skin layers regenerate, dead cells are sluffed off and lay on top of the new epidermis, Arup Indra said. This shedding of dead cells is a key cause of inflammatory skin diseases such as eczema.
“So what we really do is we try to develop very simple, non-invasive methods of identifying diseases, especially inflammatory skin diseases,” Arup Indra said.
During the formation of new skin cells, lipids and proteins are built together to form a tightly-bound barrier or wall. Arup Indra puts the skin’s lipids and proteins akin to a wall’s brick and mortar.
The lipids used and the composition of them is crucial to the process, Arup Indra said. Dead cells sit on top of this lipid and protein layer and trigger a response from the body.
“And that triggers an inflammatory reaction and helps in the onset of eczema which is very different from traditional thought that it was an autoimmune disease where the immune system is activated,” Arup Indra said.
In cases of eczema, understanding the lipid composition of the skin is important, said Arup Indra. The experiment uses a common method to record lipid makeup that is relatively painless and non-invasive.
“We do a tape stripping on any population of any age. There’s no blood drawn, no biopsy. The dead cells that come up are sufficient to give us enough material to extract lipids from them correctly,” Arup Indra said. “So we extract lipids and perform what we call a lipidomic analysis. Lipidomic analysis is essentially we look into every lipid that our skin has.”
Lipidomic analyses are useful for comparing skin lipid contents of different individuals and correlate to gene expression patterns, Arup Indra said.
“We compared them with healthy subjects and we identified that there are specific subgroups of lipids, essentially free fatty acids and ceramides that were altered for eczema patients,” Arup Indra said. “And that was very striking because we found out that the lipids were negatively correlated to disease progressions.”
As for a treatment for eczema, Arup Indra is optimistic. So far there is a huge market for eczema treatment. The most common treatment employs anti-inflammatory creams such as corticosteroids.
“We identified lipids that were altered in about 70 percent of eczema patients. So that means we can probably make a general formulation that would be available over the counter,” Arup Indra said. “The different biologics that are available for the treatment of eczema are very expensive and always have side effects.”
Traditional treatments such as corticosteroids are damaging to the skin, dehydrating and stress the epidermal tissue, Arup Indra said. Along with this, products on the market currently could have long lists of ingredients.
One of the endgoals of the experiment is a simple and all-natural topical cream that is beneficial for patients with and without eczema, Arup Indra said. It includes the lipids found to be altered in eczema patients.
“And these lipids are classified as GRAS or generally recognized as safe because they are found in specific oils,” Arup Indra said. “So why not take those lipids, put them in a nice formulation with a nice smell and color and give it to whomever. So I think that this is tremendous.”
A recent pilot study with the minimalistic formulation containing the two lipids and a base can improve dry, itchy skin and prevent water loss in a pre-clinical model, according to Arup Indra.
“This can be effective to treat people of all ages with dry and sensitive skin, as well as eczema patients,” Arup Indra said. “So as much as we are developing pre-clinical models, we are also utilizing human skin equivalents. We don’t use human volunteers, we work with the industry to generate 3D skin, like 3D printing.”
The new technology in 3D skin generation offers benefits to the research being conducted, said Arup Indra.
“It’s expensive, but the good thing is that it takes away the IRB approval and all that. So we can utilize these 3D skin equivalents in the lab and we can test the efficacy of them,” Arup Indra said. “This is a new technology that we use in collaboration with other researchers.”
Research being conducted in the Indra lab has long-term impacts, Gitali Indra said. Developments in stem cell utilization help regenerate skin in a more rapid fashion for patients, such as burn victims and others.
“Stem cells are currently used for military people because they have the capacity to regenerate. What they do is they culture these stem cells and then they can use it as a spray gun on the military wounds so the healing is much faster,” Gitali Indra said. “Also, it’s especially good for burn victims since it can reduce scar formation. It’s more important for them to get that healing quicker otherwise they will have a lot of scars. So you know for those studies it’s important we can contribute to something like that in the future where we understand which factors are important for healing.”
Wound Healing
Another investigative pathway involves skin wound healing, a biologically complicated process, Gitali Indra said.
“The wound healing process is very complex, it has multiple steps although we don’t realize when we have a scratch,” Gitali Indra said. “We think it’s going to heal in a week, but there are multiple things going on inside that people are not aware of.”
Both Arup and Gitali’s studies involve using mice models and de-identified patient samples, but study different topic areas. For wound healing, a small wound is created on the mouse’s back and monitored.
“We take samples from different stages and we analyze them for different markers,” Gitali Indra said. “We have generated a mouse model in our initial studies in collaboration with Arup Indra and Mark Leid in Pharmacy, which we published in 2012, and showed that one of the transcriptional regulators named CTIP2 has a role in the wound healing process.”
The lab procedure follows close regulations for proper animal treatment according to the National Institutes of Health guidelines, Gitali Indra said. Additionally, The Institutional Animal Care and Use Committee has approved all of the studies conducted in the lab.
“Then we generate wounds, we follow them every day to make sure they are doing well,” Gitali Indra said. “We collect samples on the days we have to collect.”
“When we were doing that we understood that the epidermis was not forming well, there is a migration defect so the cells are not migrating and we also have different stem cells represented in the skin epidermis—they are also altered in these mice,” Gitali Indra added. “It was an expression pattern of molecular markers that was not normal.”
Along with this, stem cell expression in hair follicle cells was altered, Gitali Indra said. The hair follicle structure is important to the overall skin wound healing process as it provides supplemental stem cells from the different parts of the structure.
Two mouse models were created in response to this observation: one in which the transcription factor CTIP2 in question was eliminated from the entire skin, and one where it was eliminated from hair follicle stem cells only, Gitali Indra said. The latter studies were funded by a grant from NIH to Gitali Indra.
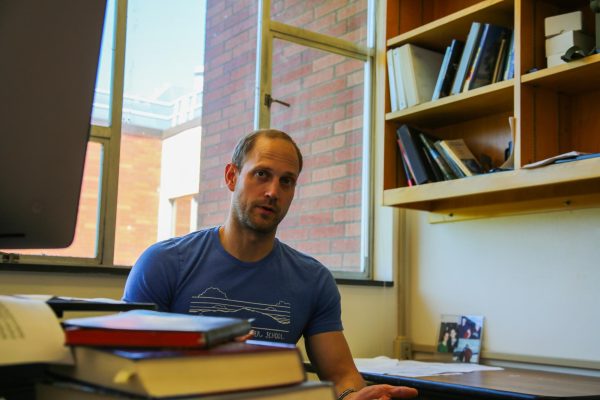
Molly Gallagher, a lab assistant in the Indra Lab, said it’s possible to generate and use genetically-modified mice to investigate certain genes that might be involved in the wound healing process.
“Often our mice have a ligand-induced enzyme introduced into their genome (Cre recombinase), as well as other slight modifications (the technical term is ‘floxing’ a gene of interest with a sequence that the Cre can identify for excision) that allow us to selectively knock out particular genes and investigate the function of that gene (and its produced protein),” Gallagher said in an email. “We can generate wounds, induce the excision of a gene of interest by applying the ligand to activate Cre, and then examine the impact of that excision to infer what role that protein might play in wound healing.”
The observations gathered from these studies create a base of knowledge that can be built upon for further experiments, Gitali Indra said.
“So these studies we think will give us an idea of what we should be doing in the future,” Gitali Indra said. “Using this mouse model, we will identify different gene expression patterns of the different factors such as growth factors, cytokines, chemokines that are produced during that wound healing environment. Those factors could be used to promote healing in burn victims, military wounds and in patients with chronic or diabetic wounds.”