OSU Department of Chemistry progresses skin cancer research
March 5, 2018
New research out of the Department of Chemistry shows promising results in anti-cancer treatments.
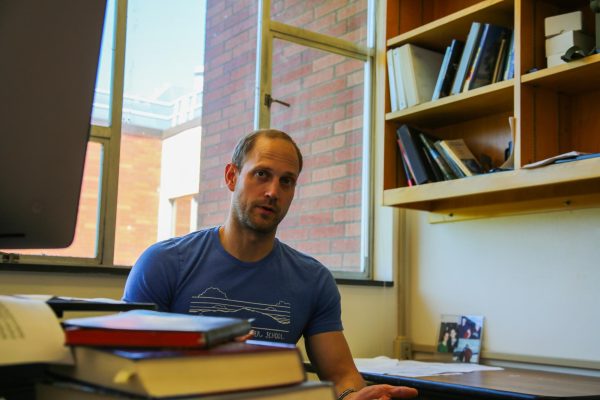
Assistant Professor Dr. Sandra Loesgen has brought mensacarcin research from the University of Göttingen to Oregon State University.
“The bacterium is from German soil. Next to the university there, and that was before 1998,” Loesgen said. “My doctoral adviser Axel Zeeck team isolated this Streptomyces bottropensis and they found mensacarcin; they could purify it and they could identify the structure.”
Graduate student Elizabeth Kaweesa looks specifically at how mensacarcin affects cancer cells.
“In determination of its cytotoxicity, it’s very selectively cytotoxic against melanoma,” Kaweesa said. “In our lab we screen compounds on colon cancer cell lines, lung cancer, breast cancer and prostate cancer but mensacarcin is very selective to melanoma and it also acts really fast.”
Kaweesa said mensacarcin induces programmed cell death, or apoptosis.
“We observe that mensacarcin enters the cell and causes cell death within 20 minutes,” Kaweesa said. “My main objective is to study the mechanism of action. We know that it does kill, but we need to figure out how it causes melanoma cell death.”
Energy metabolism in the body involves different processes like glycolysis, the citric acid cycle and oxidative phosphorylation, Kaweesa said. These reactions happen in and around the mitochondria, an organelle used specifically by cells for energy production.
“Based on fluorescence imaging and different cellular assays we know that mensacarcin targets the mitochondria; it therefore affects the energy metabolism,” Kaweesa said. “But we’re yet to figure out how it disrupts energy metabolism leading to cell death. It could be via any of the mitochondrial processes, so we’re yet to figure that out.”
Loesgen said melanoma is a unique cancer due to the body pathway it exploits for energy.
“Normally, you have (adenosine triphosphate) production done by oxidative phosphorylation. Cancers need a lot of energy; they need to grow fast,” Loesgen said. “Most of the times, the oxidative phosphorylation is highly increased to supply the energy for cancerous tissue. But in melanoma we see it’s glycemic. So it’s using a different pathway and that makes a difference.”
Glycemic means that the cancer derives its energy from glycolysis, the first step in energy metabolism, Loesgen said.
“So melanoma cancer cells are very different compared to other cancer tissues. I think it’s a big theme and we see many papers coming out where people try to utilize this metabolic weakness or difference,” Loesgen said. “So if we have molecules that could target energy metabolism that could be very selective with less side effects, I think it’s kind of a revolution right now. That way of targeting.”
Associate Professor Arup Indra in the OSU/OHSU College of Pharmacy has worked on melanoma cancers for over 20 years.
“Now melanoma is one of the deadliest skin cancers and Oregon has the 3rd highest incidence rate in the nation. Melanoma is different from squamous cell carcinoma because of the fact that squamous cell carcinomas are aggressive but they could be receptive, they could be treated with chemotherapy and surgical removal,” Indra said. “But melanomas, they often metastasize very rapidly.”
The most challenging aspect at this point is obtaining funding to go ahead with preclinical trials, Indra said.
Loesgen said that despite the promising results observed, the chances of reaching a final drug for melanoma treatment are slim.
“It takes years. It takes 15, 20 years from the stage we are at,” Loesgen said. “And the amount of compounds, I think 5-10,000, that are probably in the pool that mensacarcin is in now, one makes it (to a final product). One of 10,000. While we have the best hopes, it might not be this one.”
According to Indra, the preclinical animal models generated in his lab are unique because they contain specific gene mutations in skin cells that are found in humans. Using an animal model may overall be the most effective way to test anti-cancer efficacy of new drugs including bioactive compounds isolated from different resources.
“Mice are an ideal model where it is manageable, you can do things within a year or two. The diversity or heterogeneity is relatively less and so it’s a good fit model to do things rapidly,” Indra said. “A mouse can resemble human skin in a lot of aspects. It could be more cost effective, more controlled and it could be done in a more effective way.”
Loesgen said testing with animal models is regulated by both the National Institute of Health and the Food and Drug Administration.
“If you look into the guidelines, they’re really, really strict in how many mice need to go into an assay, the fewest possible are sacrificed in a very detailed way. This is all very regulated,” Loesgen said. “And it’s also expensive, that kind of work. So we are looking into initial efficacy and dose texploration, with only few mice per test. And the collaborators on the clinical side, they are very experienced.”
According to Indra, these preclinical studies may consider new angles of approaching melanoma treatment studies.
“These are unique in a sense because we consider the microenvironment effect,” Indra said. “What that means is the cancer and the associated effect of the environment, which is very often ignored for cells in isolation.”
Kaweesa said if a product is not generated, there are still benefits of completing the research process.
“We might not be able to develop mensacarcin as a new drug for melanoma; hopefully we can in our lifetime. Even if we do not, all the assays and protocols we’re developing, all the pathways we’re digging into provides insight on how to develop targeted cancer therapies, therefore contributing to the research world,” Kaweesa said. “And maybe other scientists, or even younger scientists in years to come will use the same techniques and develop them further.”
Furthermore, though research has been focused on melanoma it may be effective in treating other kinds of cancers, according to Loesgen.
“And it seems to be effective in glioblastoma, which is a really aggressive form of brain tumor for which it is really important to have tools,” Loesgen said. “We do not know if it carries over the brain barrier yet, so that’s something we need to study. Mensacarcin’s application in melanoma is one avenue we are exploring, but there might be other cancers, more aggressive ones.”